Key Takeaways:
- Often associated with sleep apnea, cheyne-stokes is a specific type of abnormal breathing.
- People with Cheyne-Stokes may have periods of rapid, deep breaths followed by pauses in breathing during sleep.
- This can negatively impact the quality of sleep and leave people with daytime fatigue, headaches, and more. Learn about causes, symptoms, diagnosing, and treating in this article.
Both Cheyne-Stokes and sleep apnea are respiratory conditions, but there are differences. Cheyne-Stokes respirations are a rare abnormal breathing pattern that can occur while awake but usually occurs during sleep. Cheyne-Stokes breathing may be associated with central sleep apnea.
Obstructive sleep apnea involves apneas caused by a physical blockage in the throat, usually relaxed muscle tissue. Central sleep apnea occurs when the body does not make the appropriate respiratory effort during sleep due to the absence of signals from the brain.
What are Cheyne-Stokes?
Cheyne-Stokes respiration is a condition that causes abnormal breathing during sleep. This abnormal breathing often includes “apneas,” or periods of stopped breathing, which explains why the condition is so frequently referenced in sleep apnea medical circles.
These apneas occur because Cheyne-Stokes respiration generally causes a person’s breathing to follow abnormal patterns or dysrhythmias. This means that breathing gradually increases and decreases during sleep. These cycles of increasing and decreasing breathing activity ordinarily last from 30 seconds to two minutes in duration, with five to thirty seconds of apneas.
Why Do Cheyne-Stokes Respirations Happen?
Breathing is how the body takes in oxygen and releases carbon dioxide. While a person is asleep, the respiratory center, a part of the brain, is what regulates their breathing. Cells within the arteries will send a signal to the respiratory center about the levels of oxygen and carbon dioxide in the blood. The brain will then use these signals to control the muscles that help a person breathe. Cheyne-Stokes breathing happens because of a delay in the brain’s detection of the level of carbon dioxide in the blood. This delay will affect the normal cadence of breathing.
In Cheyne-Stokes respirations, the delay in signals limits the brain’s ability to maintain a steady rate of breathing. Breathing will become faster to reduce the carbon dioxide in the blood, which then could result in too low of carbon dioxide levels. Because of this, breathing will slow or stop, restarting this cycle.
Causes Of Cheyne-Stokes
The most common causes of Cheyne-Stokes respirations are heart failure and stroke. Although considered to be rare, Cheyne-Stokes breathing occurs in 25% to 50% of people with heart failure. This breathing pattern appears less common in people who have suffered a stroke than in those with heart failure, though factors like the involvement of a major artery may increase the risk. Other causes include:
- Arrival at a high altitude
- Brain injury or brain tumor
- Kidney failure
What is Sleep Apnea?
Sleep apnea is a common sleep condition in which your breathing stops and restarts many times while you sleep. This can prevent your body from getting enough oxygen. Chronic sleep apnea leads to sleep deprivation which can affect both your physical and mental health. Obstructive sleep apnea is the most common type and relates to the blockage of the airway. Central sleep apnea is less common and relates to brain signals to the airway muscles.
Causes of Sleep Apnea
In adults, the most common cause of obstructive sleep apnea is excess weight and obesity, which is associated with the soft tissue of the mouth and throat. During sleep, when throat and tongue muscles are more relaxed, this soft tissue can cause the airway to become blocked. Age is also a factor, as older adults tend to experience obstructive sleep apnea as well. In some cases, heredity and the development of the throat muscles and tissue may be the cause of sleep apnea.
How Do Cheyne-Stokes Respirations Differ From Similar Breathing Disorders?
Cheyne-Stokes is similar to another breathing disorder called Kussmaul, which is characterized by fast breathing and too much carbon dioxide in the body. However, Kussmaul’s breathing doesn’t alternate between fast and slow breathing or cause breathing to stop as Cheyne-Stokes does.
Cluster breathing, also known as Biot’s respirations, is similar to Cheyne-Stokes because it involves groups of rapid, shallow breathing, after which periods of apnea then follow. However, it does not involve cycles of deep breathing or gradual changes in breathing patterns as Cheyne-Stokes does.
Symptoms Of Cheyne-Stokes vs. Sleep Apnea
Cheyne-Stokes
Cheyne-Stokes sleep and respiratory symptoms are often very similar to those of sleep apnea. These patterns of symptoms can often lead to a misdiagnosis. Doctors must look closely at the root cause of certain symptoms to detect differences between a Cheyne-Stokes diagnosis and that of sleep apnea.
Common symptoms of this condition include:
- Fatigue and excessive daytime sleepiness
- Difficult or labored breathing
- Loud snoring ( usually detected by a bed partner)
- Sudden coughing fits
- Periodic limb movements during sleep
Sleep Apnea
Because obstructive sleep apnea is prevalent, doctors may be quick to diagnose Cheyne-Stokes as sleep apnea. While there is a similarity in the symptoms between the two sleep conditions, they are slightly different when it comes to treatment. Sleep apnea symptoms include:
Loud snoring, episodes in which you stop breathing during sleep — which would be reported by another person, gasping for air during sleep, awakening with a dry mouth, morning headache, difficulty staying asleep, known as insomnia, and excessive daytime sleepiness, known as hypersomnia.
Difference Between Sleep Apnea And Cheyne-Stokes Breathing
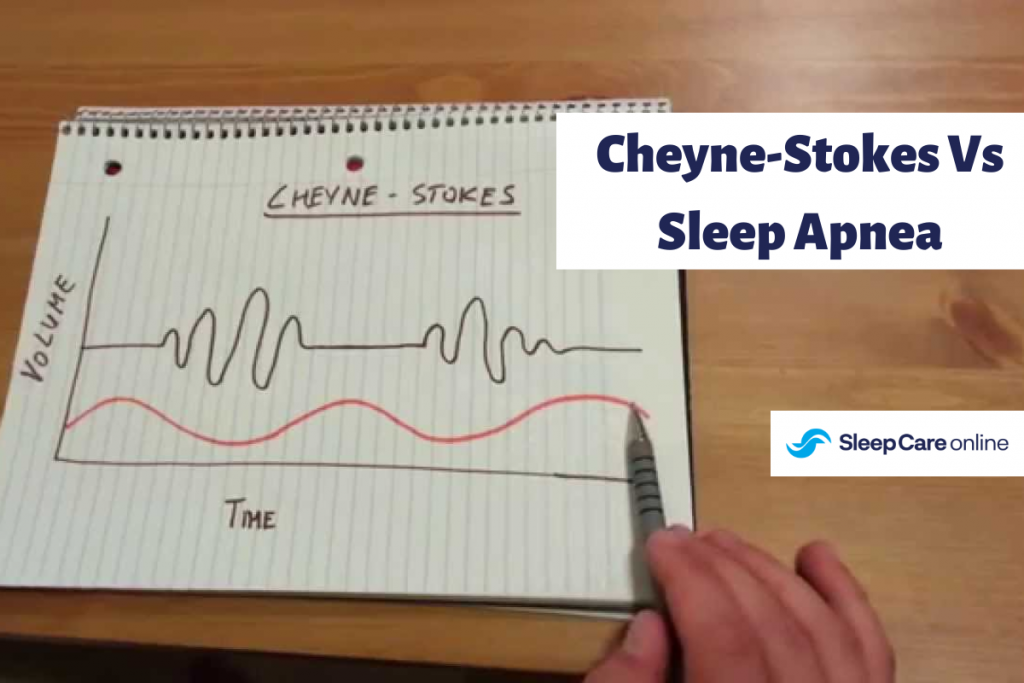
One of the key differences between sleep apnea and Cheyne-Stokes is the pattern of breathing that the patient experiences. Cheyne-Stokes follows a cyclical interruption in breathing. The patient will breathe normally for a period of time and then cease breathing for a period of time. These cycles repeat throughout the night. Sleep apnea interruptions in breathing tend to be more erratic and do not follow any pattern.
Doctors who suspect one condition over the other will pay attention to the pattern of breathing in a sleep study to make an accurate diagnosis.
Diagnosing Cheyne-Stokes vs. Sleep Apnea
Cheyne-Stokes
Cheyne-Stokes is usually diagnosed in an in-lab sleep study rather than with a home sleep test. Sleep doctors and technicians must carefully observe the patient to detect noticeable patterns in the breathing that indicate Cheyne-Stokes. The cyclical breathing pattern involves periods of ceased breathing followed by periods of respiration that can last between 30 seconds to two minutes in duration.
By observing these cyclical breathing patterns, doctors will know that the patient has Cheyne-Stokes rather than sleep apnea.
Sleep Apnea
Sleep apnea is diagnosed by more erratic periods of breathing. There is no set pattern that a doctor can observe, which may lead a doctor to diagnose the sleep disorder as sleep apnea. Doctors will most likely look for frequency in the periods of ceased breathing to determine the severity of the sleep apnea. Sleep apnea, unlike Cheyne-Stokes, can be diagnosed accurately in a home sleep apnea test as well as with an in-lab sleep study.
Check out Sleep Care Online as a convenient, safe, and affordable way to get tested for sleep apnea in the comfort of your own home. This test was designed to fit into a person’s lifestyle as it doesn’t require going into a lab for testing.
Treating Of Cheyne-Stokes vs. Sleep Apnea
Treatment for Cheyne-Stokes
Cheyne-Stokes may be treated in a number of ways. Respiratory stimulants or depressants may be prescribed to help regulate normal breathing, either by speeding it up or slowing it down. Oxygen therapy may also help to keep breathing consistently while the patient sleeps and help prevent periods of ceased breathing. CPAP therapy is also a common treatment as it can help control and modify erratic breathing, but it is not the choice most doctors prescribe. Other treatment options include:
- Bilevel positive airway pressure (BiPAP): Bipap is another form of PAP therapy, but the machine increases the pressure of the stream of air during inhalation and decreases the pressure during exhalation. BiPAP may be recommended when CPAP or supplemental oxygen therapy isn’t effective in normalizing nighttime breathing.
- Adaptive servo-ventilation: ASV is an advanced form of PAP therapy that assesses breathing in real time and adjusts pressure accordingly. ASV may be used in some people with central sleep apnea but is not recommended for some individuals with heart failure.
- Nerve stimulation: Phrenic nerve stimulation is a treatment for central sleep apnea in which a medical device is implanted in the body to regulate breathing. The device affects breathing by stimulating the phrenic nerve, which causes the diaphragm to contract. Nerve stimulation is typically reserved for when other treatments aren’t successful.
Treatment for Sleep Apnea
Sleep apnea is most commonly treated using CPAP therapy. CPAP, or continuous positive airway pressure, uses a machine to pump pressurized air through a hose and into a mask that the patient wears while they sleep. The pressurized air helps keep the airway open during sleep and prevents the interrupted breathing characteristic of sleep apnea.
Other solutions such as BiPAP and APAP devices can also help with nighttime respiration if CPAP does not prove successful with a patient.
Conclusion
If you notice you are experiencing any of the symptoms of sleep apnea, it is important to get tested for this sleep disorder as soon as possible. Sleep Care Online offers a safe, simple, and affordable way to get tested from the comfort of your own home. Learn more about Sleep Care Online here!

Dr. Kunal Agarwal is a highly accomplished board-certified physician specializing in Family Medicine, Sleep Medicine, and Obesity Medicine. He completed his residency at Michigan State University and a fellowship at Henry Ford Health System, and has over a decade of experience delivering exceptional patient outcomes. Dr. Argarwal is passionate about patient education and advocacy, sleep disorders, and more. His expertise in treating sleep apnea is extremely valuable to improve his patients’ lives.
Awards, Honors, & Recognition
Top Doctor
SRQ Magazine and Sarasota Magazine, 2023-2024
Fellow of American Academy of Sleep Medicine (FAASM)
American Academy of Sleep Medicine, 2021
Named “Top Doctor” for 2017, 2018 (on cover), 2019,and 2020 by Delaware Today Magazine
2017-2020




