Key Takeaways:
- One of sleep apnea’s most common symptoms for individuals is headaches in the morning after waking up.
- This can be due to a poor night’s sleep from continuous disruptions in the sleep cycle caused by sleep apnea.
- There are a few different types of headaches that are associated with sleep apnea symptoms, and simple lifestyle changes that can reduce headaches. Learn more in this post by Sleep Care Online.
Sleep apnea and headaches, especially recurring headaches are linked. Some people with obstructive sleep apnea (OSA) experience these headaches upon waking up, at least 15 days per month. They are characterized by a pressing, not pulsing, pain that is usually felt across both sides of the head and can last up to four hours. Unlike some other types of headaches, sleep apnea headaches are not accompanied by nausea or sensitivity to light and sound. People with OSA may be up to three times more likely to experience morning headaches.
Can Sleep Apnea Cause Headaches?
Obstructive sleep apnea can, over time, reduce blood oxygen saturation in the bloodstream. That means less oxygen is reaching various parts of the body, including the brain. Consistent poor sleep from sleep apnea can lead to consistent morning headaches as the brain receives less oxygen. The brain is literally reacting to oxygen starvation with pain. Along with oxygen deprivation, sleep apnea episodes can also increase carbon dioxide, which can cause the brain to swell and add to the pain.
What are Sleep Apnea Headaches?
Severe headaches are so common among sleep apnea patients that they are characterized as sleep apnea headaches. The intense pain is unique from other types of headaches and is felt upon waking. The pain can last for hours and the consistency of the headaches in the morning are the first sign that sleep apnea is causing the symptom. Other symptoms related to sleep apnea headaches include dry mouth, daytime drowsiness, and the sense of feeling unrefreshed even after a full night’s sleep.
What Does A Sleep Apnea Headache Feel Like?
Sleep apnea headaches tend to occur in the morning right after you wake up, but it is not rare to wake up with one in the middle of the night, either. Sleep apnea headaches feel like pressing pain, not pulsing, on all sides of your head. It can last from 30-4 hours but are receptive to treatment.
What are the Risks Related to Sleep Apnea Headaches?
Sleep apnea headaches are most common among female sleep apnea patients. Also having a history of headaches in your past may increase the tendency. Those with moderate to severe obstructive sleep apnea are more likely to experience sleep apnea headaches. As sleep apnea worsens among some patients the severity and frequency of sleep apnea headaches may also increase.
As patients with mild sleep apnea remain undiagnosed and untreated, the likelihood of sleep apnea headaches occurring and getting worse may become a problem.
Overall, sleep apnea risks include:
- Obesity
- Other medical conditions that may cause sleep apnea
- Smoking or regular alcohol use
- Aging
- A family history of obstructive sleep apnea
Many sleep apnea patients, especially those who go undiagnosed, may try to self-medicate sleep apnea headaches with over-the-counter medications. The importance of getting diagnosed with sleep apnea becomes more essential when painful symptoms like sleep apnea headaches start to impact daily life and health.
Types Of Headaches Linked with Obstructive Sleep Apnea
Cluster Headaches
Cluster headaches are associated with sleep apnea symptoms, but they are distinct from sleep apnea headaches. They tend to occur during sleep, whereas sleep apnea headaches occur upon waking up. Also, unlike sleep apnea headaches, cluster headaches often include additional symptoms like a runny or stuffy nose, tearing up of the eyes, sweating on your forehead or face, and puffy or droopy eyes.
Cluster headaches often occur in clusters. For example, you may experience a few headaches a day, always around the same time, for a period of a few months. Then, you may not have any until the following year. Cluster headaches last around an hour on average.
Migraines
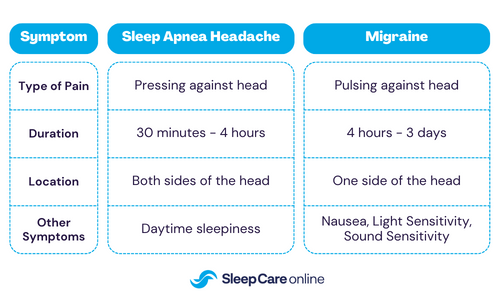
Sleep apnea headaches are different from migraines. Migraines tend to last much longer, between four hours to three days, while a sleep apnea headache usually goes away on its own within a few hours of waking up. You may feel a sleep apnea headache on both sides of your head, while a migraine is typically only on one side.
Also, migraines can occur any time of day or night, including during sleep, while sleep apnea headaches occur upon waking up. Unlike sleep apnea headaches, migraines typically have other symptoms, such as nausea or sensitivity to light and sound.
Hypnic Headaches
Hypnic headaches, which also occur at night, are another sleep-related headache that may affect people with obstructive sleep apnea. They are more common among older people. While sleep apnea headaches begin after you wake up, hypnic headaches generally begin about four to six hours after falling asleep and often cause a person to wake up. This is why they have earned the nickname of alarm clock headaches.
Like sleep apnea headaches, hypnic headaches usually go away on their own within 30 minutes to an hour, but they have additional symptoms like nausea, which is not the case with sleep apnea headaches.
Sleep Apnea Headaches vs. Migraines
Causes Of Sleep Apnea Headaches
Because sleep apnea reduces blood oxygen levels in the bloodstream, the likelihood that limited oxygen is reaching the brain may be the reason behind sleep apnea headaches. The lapses in breathing that characterize sleep apnea can cause lower blood oxygen levels during sleep. This allows less oxygen to reach the brain and causes carbon dioxide to accumulate in the bloodstream, whereby blood vessels in the brain expand. As the pressure from that expansion builds up, it may develop into a sleep apnea headache and cause pain.
Some research has suggested that sleep apnea episodes may contribute to high blood pressure and cardiovascular disease, which can contribute to sleep apnea headaches.
Whether sleep apnea headaches stem from reduced oxygen levels or health side effects, it is clear that sleep apnea causes sleep deprivation which has a dramatic impact on overall health.
How Are Your Morning Headaches Caused by Sleep Apnea?
Peaceful and healthy sleep allows the brain and body to rest and recharge. Sleep apnea causes interruptions in normal breathing patterns as you sleep. The airway closes causing periods of choking and gasping for air that may occur frequently throughout the night. With the increased frequency of these episodes, the person suffering from the condition loses sleep every night.
With sleep deprivation come a host of symptoms from daytime drowsiness to painful morning headaches. Nightly reduced oxygen supply to the brain starts to reduce the ability of the brain to renourish and recharge and may leave carbon dioxide in the brain which aggravates headaches.
During the day, the body and brain are deprived of sleep, and never fully recover from the previous day’s activities. Long-term sleep loss has lasting impacts on the brain and body, and headaches in the morning are a warning sign that your brain is oxygen-starved.
How Can You Treat Headaches Caused by Sleep Apnea?

Change In Lifestyle
Many lifestyle choices can affect healthy sleep and contribute to sleep apnea headaches. Avoiding alcoholic beverages can help you get the sleep you need. If you do not want to quit alcohol entirely, avoiding alcohol before bedtime can help reduce sleep apnea symptoms and the possibility of headaches in the morning.
Smoking can also narrow blood vessels which can inhibit healthy sleep and play a role in morning headaches. Quitting smoking is a big step toward gaining healthier sleep and reducing sleep apnea headaches.
CPAP Therapy
If you have received a sleep apnea diagnosis, your doctor may prescribe CPAP therapy as a treatment. CPAP therapy involves the use of a CPAP machine with directs pressurized air through a hose and into a CPAP mask. This constant flow of air keeps the airway open all night long so that you do not experience sleep apnea during the night.
With consistent CPAP compliance, many patients may find that they have healthier, better sleep and feel more energized during the day. They will also see a dramatic reduction in sleep apnea symptoms including sleep apnea headaches.
Surgery
For some patients with sleep apnea, the problem may not go away with CPAP therapy. Some patients may have irregularities in their throat muscles or airway which may be causing their sleep apnea. Surgery may be the best option to correct the anatomical problem. Sleep apnea patients who have tried CPAP therapy without positive results may have to resort to surgery. Once corrected, the airway will remain open and allow the patient to sleep peacefully without sleep loss or sleep apnea headaches in the morning.
Oral Appliance
For other sleep apnea patients, a simple oral appliance worn at night may be enough to curb sleep apnea episodes. Some mild to moderate cases of sleep apnea may not require the use of CPAP therapy with a CPAP machine. The use of an oral appliance can correct anatomical issues that allow the airway to naturally remain open and reduce sleep apnea episodes and morning sleep apnea headaches.
Speak to your doctor about the best solution for managing your sleep apnea after diagnosis.
When to Consult a Doctor
If you have any of the typical sleep apnea symptoms including morning headaches, it is probably time to speak with a doctor about your symptoms. Your doctor may ask questions such as:
- Are your morning headaches frequent?
- Do you snore loudly at night?
- Are you waking up gasping for air at night?
- Do you feel drowsy or unrefreshed during the day even after a full night’s sleep?
If you answer yes to these questions, your doctor may recommend a sleep apnea test.
How Can I Diagnose Sleep Apnea at Home?
Speak to your doctor about getting tested for sleep apnea. In-lab sleep studies are one way to test for sleep apnea. However, in-lab studies require an overnight stay in a sleep lab, and may not be the most comfortable.
For convenience, you can also take a sleep apnea test at home. Sleep Care Online offers at-home sleep tests that deliver the same accurate results as in-lab tests but in the comfort of your own home. Get a diagnosis with a home sleep test today.




